#266 – Finding Hope in Uncertainty: Zoila Ortiz on her Battle with Breast Cancer and Resilience in the Face of Adversity
Welcome back to another episode of the Spun Today podcast! It's your host Tony here, and today we have a very special guest and topic to discuss with you.
In this episode, we're going to be sharing the incredible story of my wife Zoila and her recent battle with breast cancer. Zoila, underwent a hysterectomy last year and was subsequently diagnosed with early stage breast cancer around the holidays.
Zoila's story highlights the vital importance of early cancer detection, having a strong support network, and maintaining hope in the face of adversity. Her ability to stay positive, express gratitude, grace, and find moments of calm during such a difficult time is truly inspiring.
In our conversation, we discuss the physical and emotional impact of her surgeries and treatments, as well as the love and support she received from family, friends and coworkers. Zoila also shares her advice for others who may be going through similar challenges.
This episode is a poignant reminder to cherish our health, our loved ones, and the precious time we have. It's a call to approach the obstacles in our lives with courage, perspective and appreciation for what matters most.
So join me for this special episode as we hear Zoila's incredible story of perseverance. It just may change the way you think about confronting challenges in your own life and inspire you to be a source of strength for others during their trying times.
Thank you for listening in to this very special episode of Spun Today. We'll be back with more soon.
The Spun Today Podcast is a Podcast that is anchored in Writing, but unlimited in scope. Give it a whirl.
Twitter: https://twitter.com/spuntoday
Instagram: https://www.instagram.com/spuntoday/
YouTube: https://www.youtube.com/@spuntoday
Website: http://www.spuntoday.com/home
Newsletter: http://www.spuntoday.com/subscribe
Links referenced in this episode:
Check out the episode page for more content from the episode: https://www.spuntoday.com/podcast/266
BRCA (Gene Test Info): https://www.cancer.gov/about-cancer/causes-prevention/genetics/brca-fact-sheet
Cold Cap Therapy: https://paxmanscalpcooling.com/
Follow Zoila on YouTube: @zoilarosa1211
Zoila’s MS episode: #042 – Multiple Sclerosis https://www.spuntoday.com/podcast/042
Get your Podcast Started Today! https://signup.libsyn.com/?promo_code=SPUN
(Use Promo code SPUN and get up to 2-months of free service!)
Check out all the Spun Today Merch, and other ways to help support this show! https://www.spuntoday.com/support
Check out my Books
Make Way for You – Tips for getting out of your own way
Melted Cold – A Collection of Short Stories
http://www.spuntoday.com/books/ (e-Book, Paperback & Hardcover are now available).
Fill out my Spun Today Questionnaire if you’re passionate about your craft. I’ll share your insight and motivation on the Podcast: http://www.spuntoday.com/questionnaire/
Shop on Amazon using this link, to support the Podcast: http://www.amazon.com//ref=as_sl_pc_tf_lc?&tag=sputod0c-20&camp=216797&creative=446321&linkCode=ur1&adid=104DDN7SG8A2HXW52TFB&&ref-refURL=http%3A%2F%2Fwww.spuntoday.com%2Fcontact%2F
Shop on iTunes using this link, to support the Podcast: https://itunes.apple.com/WebObjects/MZStore.woa/wa/viewTop?genreId=38&id=27820&popId=42&uo=10
Shop at the Spun Today store for Mugs, T-Shirts and more: https://viralstyle.com/store/spuntoday/tonyortiz
Background Music: Autumn 2011 - Loxbeats & Melody - Roa
Outro Background Music: https://www.bensound.com
Spun Today Logo by: https://www.naveendhanalak.com/
Sound effects are credited to: http://www.freesfx.co.uk
Listen on: iTunes | Spotify | Stitcher | Pocket Casts | Google Podcasts | YouTube | Website
transcript
Zoila [00:00:00]:
Yeah, we got the results. We have my chart, and we read it, but we didn't understand.
Tony [00:00:05]:
Yeah, we didn't. It was in the, you know, medical jargon, so we started googling, which we didn't do.
Zoila [00:00:10]:
Yeah. Which is googling, which we didn't get any answers anyways.
Tony [00:00:15]:
I don't. We didn't get any clear answers, but it did seem like it was cancerous.
Zoila [00:00:19]:
Mm hmm.
Tony [00:00:20]:
Which was scary, obviously.
Zoila [00:00:22]:
And we had to wait until the holidays were overdeveloped. And I kept on messaging the oncologist, like, oh, can you just call me? Just tell me the result, because I can't wait until, like, the following week or whatever.
Tony [00:00:39]:
Yeah.
Zoila [00:00:40]:
But she was. She was like, no, I want to see you. I was like, okay, that's not a good sign.
Tony [00:00:45]:
Yeah.
Tony [00:01:04]:
What's up?
Tony [00:01:05]:
What's up, folks?
Tony [00:01:05]:
What's going on? Welcome to the Spun Today podcast, the only podcast that is anchored in writing but unlimited in scope. I'm your host, Tony Ortiz, and I appreciate you listening. This is episode 266 of the Sponsor Day podcast. And in this episode, my lovely wife Zoila, joins us once again. She's a sponsorialum. She's been on the podcast in the past, this time, unfortunately, on a sadder note than usual, but a hopeful one at the same time. I've alluded to the contents of this episode during prior episodes, where I've said that there's a reason why I've been re releasing more episodes than normal this year, like, putting out the throwback episodes. But I didn't really want to get into the details of it all until and when this episode came to fruition.
Tony [00:01:53]:
So earlier this year, actually towards the tail end of last year, as we'll get into during the episode, my wife was diagnosed with breast cancer. So this entire episode is essentially documenting and reliving all the moments from initial testing and diagnosis. What led up to it, a couple surgeries that she had to have, toughing through chemotherapy, and the eventual light at the end of the tunnel. All heavy topics, but I promise you, it's more of a hopeful episode than a sad, depressing one. In short, they caught the cancer super, super early, and she's successfully gone through all the protocols that she's had to go through yet to go through twelve chemo sessions. When we recorded this, it was actually, she was done with her 10th, so she had two more to go since then. She completed those two like a champ, and next week, actually has her final and reconstruction surgery. And thereafter, it's just a matter of regular visits.
Tony [00:02:50]:
With her doctors, her oncologist, just to stay on top of things. But the expectation, obviously, is that she won't have to deal with any of this again. And I want to highlight here, right in the intro, because my goal for this episode, aside from documenting it for our family and our children to listen to in the future when they're old enough to understand what their mom went through, is to spread awareness and also to give folks that may be going through a similar situation hope that there is light at the end of the tunnel. They can definitely get through something like this. But I want to highlight mainly, and we get into it throughout the episode, but a few minutes into it, so I want to make sure I highlight it. Here in the intro as well, is the BRCA gene testing, which is what essentially saved my wife's life. So I was peripherally aware of what this was because my wife had done the BRCA gene test and told me about it, I think something like ten years ago or something like that, nine or ten years ago. And what it is, is a gene test.
Tony [00:03:49]:
And my understanding is that it's normally given to women or folks that. And I think women specifically, actually, although don't quote me on that, that have a family history of cancer, mainly like breast cancer, ovarian cancer. And my wife's mom passed of ovarian cancer many years ago. So a doctor had her and her sisters do this BRCA gene test way back then. And the idea is that it tells you and gives you percentages of, if you're predisposed to developing cancer and fairly accurately, it can predict this, and it gives you percentages of how likely you are to develop ovarian cancer or breast cancer. And I believe pancreatic cancer as well, or if you're not predisposed, if you don't have the gene for it. Now, back when they did the test, I want to say, like, which is a really, really important point that I want to. That I want to make here.
Tony [00:04:40]:
Back when they did the test ten years ago, they were all negative for it in my mind. And I mentioned this in the episode, I figured, you know, your genes are your DNA, or, like, I think of DNA when I think of genes, right? And I figure, like, whatever you're born with is what you have for life. Like, it never changes. And that may be the case, however, the. And I'm not sure if that's the case or not, by the way, but the point is that the testing that we have, the science that we have to test different genes and different gene expressions or whatever it is. The BRCA test is doing changes over time, it gets more. More sophisticated, more advanced. So now when she did the BRCA gene test, she did test positive.
Tony [00:05:18]:
So I say that to say, mainly, if you've ever done the BRCA gene test and you already know what it is and it's been years, do another one because you never know. So she was negative, like ten years ago, thought it was something that she never had to worry about, but she didn't have the results or something like that. So the doctors had her do another one. And we'll get into the reasoning why during the episode. But essentially, this one came back positive and she had a very, very high chance of developing ovarian cancer. 60% chance, I believe it was, and like a 40% chance of developing breast cancer. And that led us into the surgeries, one of the surgeries that she did. And then during the follow ups that they put her on every three to six months for, like, breast imaging just to make sure nothing's going on, she passed her mammal and sonogram.
Tony [00:06:04]:
That didn't pick up anything. Which is another thing I'd like to highlight. You know, definitely, ladies out there, do your mammograms on a routine basis. You know, book your appointments around your birthday. That's a good way to remember, like, your physical, your mammals and you, you know, whatever you got to do. But also, that didn't pick up anything. But because of that BrCA gene test, they also sent her to do an MRI, and then that is what picked up the cancer. Had she not done that and just waited, another year would have been growing and spreading inside of her with no detection, essentially.
Tony [00:06:33]:
So, yeah, I just definitely, definitely want to highlight the importance of doing that BrCA gene testing. B r A C A. I'll see if I could link to something related to it in the episode notes for folks to check out the. And again, in the episode, we're going to get into more details about it, but I wanted to make sure that folks hear that from the very beginning of this episode. Then just want to mention a few other things before we jump in that were not covered in the episode. But first and foremost, a huge, huge, huge thank you to all our family and friends for the outpouring of support, our co workers on both sides. You know how they say it takes a village to raise a kid? It definitely takes a village when families going through tough times like these. From my mom, who's always been a rock in every situation, always there, who last year went through her own cancer scare, breast cancer as well, but had a very, very rare type zero, they.
Tony [00:07:27]:
Called it, because it was a completely.
Tony [00:07:29]:
Encapsulated something or another. I forget the medical terminology for it, but it was completely encapsulated type zero breast cancer. She had a lumpectomy, a couple rounds of radiation, and the entire time was just like, that wasn't cancer. To my brother and sister in law.
Tony [00:07:48]:
Always there to take the kids for.
Tony [00:07:50]:
A few hours while I helped Soyla deal with things. To Soyla's sisters, same thing. Come over here, cook for us. To my aunts and uncles and cousins, just like, constantly calling, checking in, sending gifts, my coworkers as well, which, honestly, and I'd be remiss if I didn't. If I didn't mention this. I never even thought of this as a thing, but of course, it is one. Like, in, you know, hindsight is 2020, but, like, my coworker sent a, like, a very generous Grubhub gift card, and they sent, like, gifts for the kids to, like, distract them, like, toys and stuff like that. And the sentiment behind the gift card is like, listen, you guys are going through all of this, and, you know, if this could alleviate having to figure out, like, what you guys are gonna order for or have for food and cooking and stuff like that, then, you know, that's what it's for.
Tony [00:08:40]:
And it was so clutch. It was something that I would never even think of or hadn't before, but came in definitely so handy. So thank you very much to each one of them, cousins as well, that send gifts, other friends that send gift.
Tony [00:08:51]:
Cards for other food places.
Tony [00:08:53]:
It's truly, truly a blessing to have each and every one of them in our lives and really appreciate their support. So thank you. Thank you, thank you. And it's also not lost on me how fragile this type of situation is and how it could have gone left. These things are unpredictable. These situations are. And early detection is absolutely the strongest tool we know of to fight against something like this. It's not lost on me that a month ago, June 30, my uncle passed away.
Tony [00:09:22]:
Rest in peace. To Miki from cancer as well. He had a battle with it over five years ago, a different type of cancer, lymphoma at the time, and then it came back in the form of leukemia before even beginning to be able to do chemo. This time around, he contracted a virus, E. Coli, because his immune system was so weak, and it was too weak to even start the chemo. And unfortunately, he passed. And I say that again, just to highlight the unpredictable nature of these types of situations and I, the importance of early detection and also appreciating what we have when we have it. Health definitely is wealth, as corny and cheesy as that sounds.
Tony [00:10:04]:
Oh, and something that I thought was a great touch that we didn't mention during the episode is that while Soyla's getting chemos, her chemo sessions, you know.
Tony [00:10:14]:
It'S like a long day.
Tony [00:10:15]:
The process essentially is like, you go in like at 708:00 in the morning, you get blood drawn. Then you go upstairs, go see the oncologist to review those blood results, to see how your levels are doing, you know, how your body is doing to the chemo. Because if you get depleted enough, they have to do like blood transfusions and to pretty much, you know, check in on how you've been over the past week since your prior chemo session. Then after that, then you go upstairs to get a few hours of chemo. When you're there in the floor where you're getting the chemo infusions, the people are so nice, all the staff, all the, they're like energetic, happy, not grumpy medical type staff folks. It's like they, personality must be a requirement to work there is, in my opinion, because everybody was so super sweet and nice and helpful. And they get you warm blankets that they have this machine that warms up blankets. They have snacks, waters, sodas, coffees, pretzels, cookies, the whole nine something that was great that they had was a massage therapist that would come each time we were there and do massages.
Tony [00:11:26]:
You know, you could get your arms massaged, some nice creams and lavender oils or whatever it is that they use. And you could choose like a back and neck massage or legs. And Soyla would always do her arms.
Tony [00:11:39]:
I just thought that was such a like dope touch.
Tony [00:11:41]:
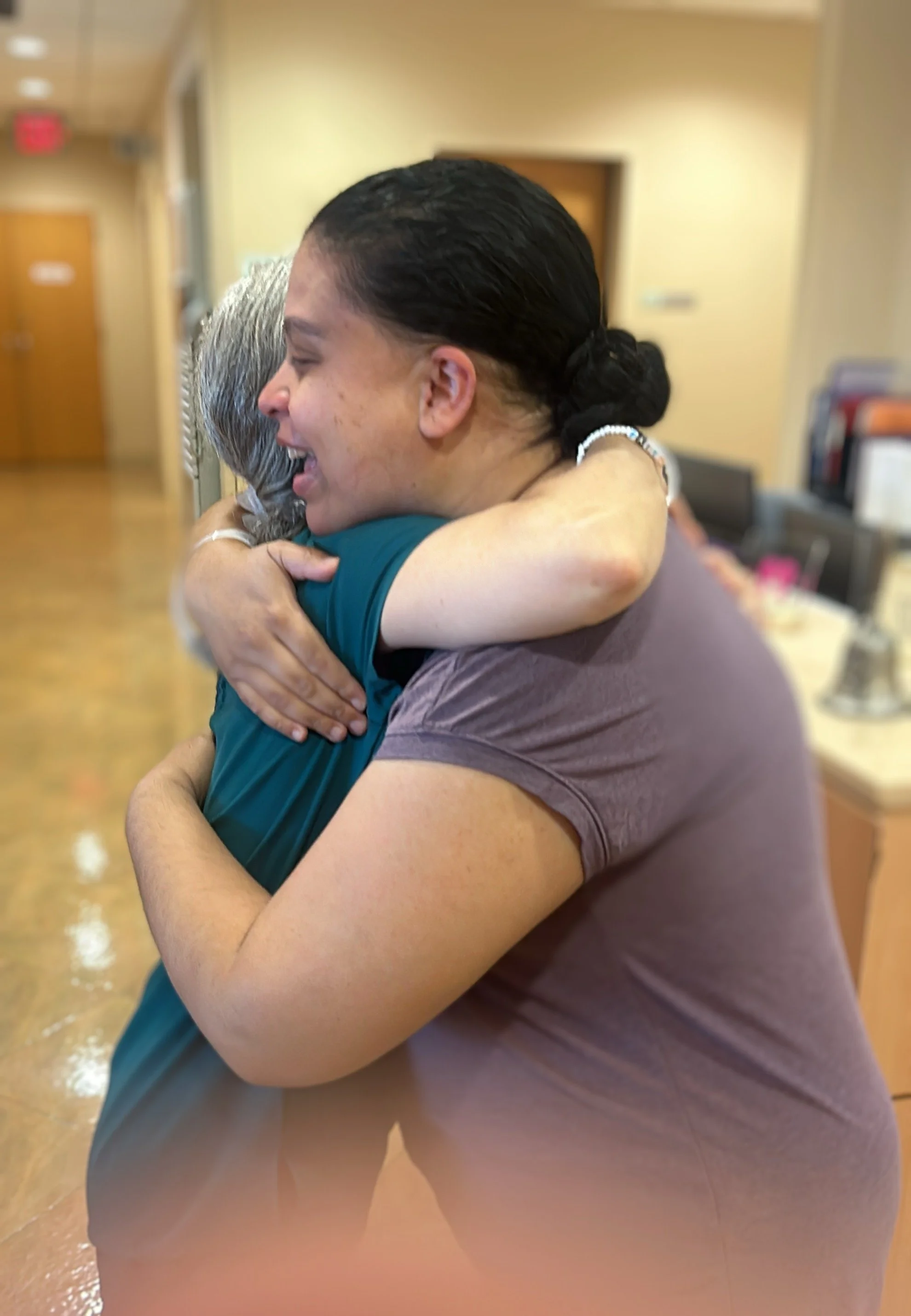
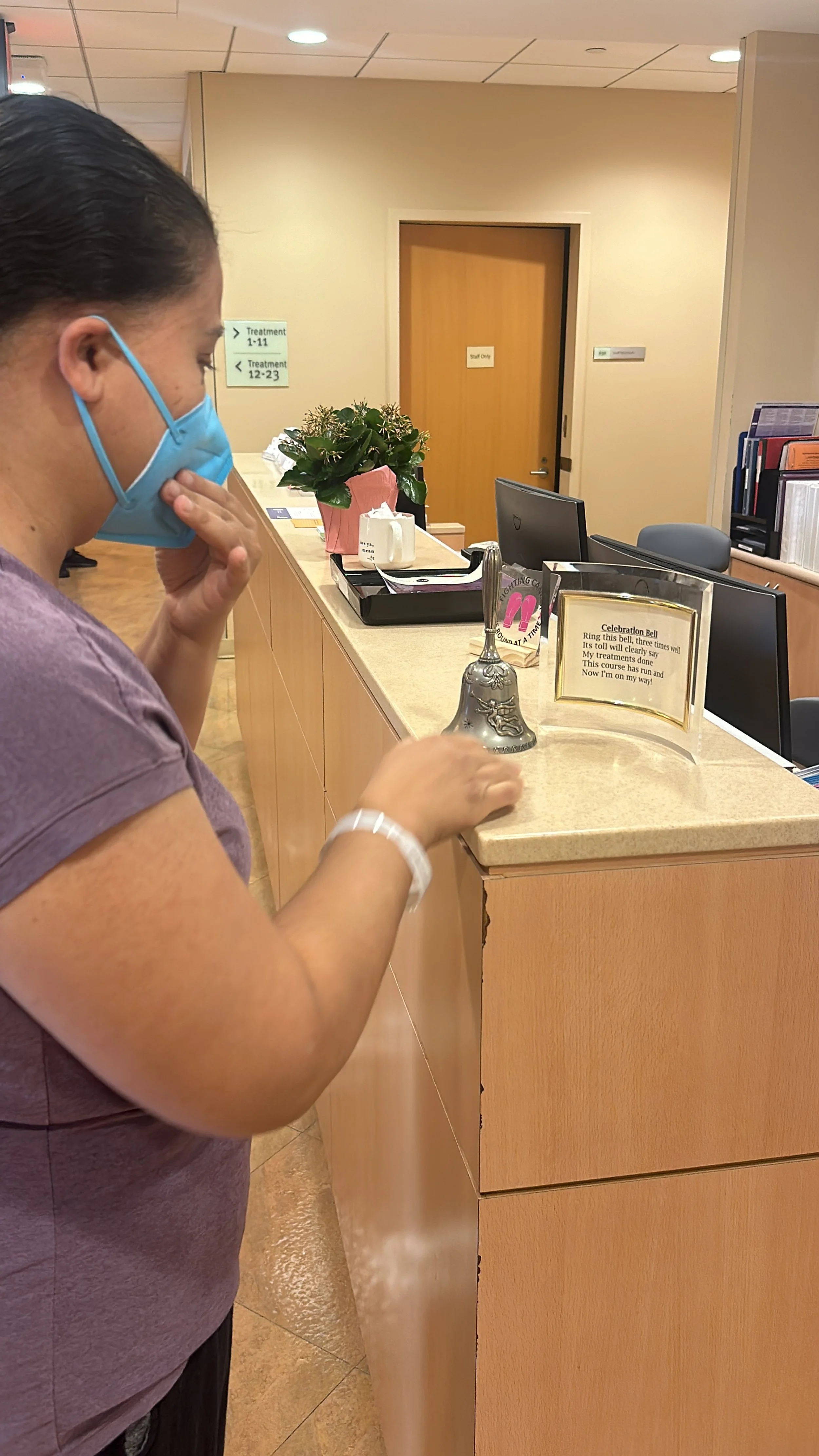
And she, you know, it was really comforting and she really enjoyed it. And they definitely do do the, you know, like ringing the bell at the end when you finish all twelve chemo sessions and it's like a really emotional moment. Everybody, you know, like all the nursing staff and stuff like that just like surround her and she reads off of a little post that they have there and rings the bell. You know, everybody's like crying and hugging. It was so super sweet, super emotional, very, very nice. And I'll see, actually if Soyla's okay with it, I'll post it to the webpage for this episode, which would be sponsored.com podcast forward slash 266. And I plan to post a couple other pics. Like for example, the cold cap therapy that we speak about in this episode.
Tony [00:12:29]:
Like I'll show you guys like with.
Tony [00:12:30]:
The machine and what the cap looks like and stuff like that. If you guys want to go check that out on the website. That was super cool and helped Soyla keep the majority of her hair. And it's something that we didn't know even existed before going through this process. It's called the cold cap therapy. Highly, highly recommend. It doesn't work on everyone. Thankfully, it did work with her, but I think it's definitely worth a shot.
Tony [00:12:52]:
And lastly, I'd say that I'll also link in the episode notes to a prior episode, one of the prior episodes that Soyla did here on the Spun today podcast, speaking all about Ms multiple sclerosis, which she has. We did that episode years ago. Just her experiences with dealing with that. Yet another thing that she's gone through, which is why I always tell her that she's the toughest girl I know. And I just want to thank my lovely wife once again. Thank you babe, for coming on the podcast. I really appreciate it. I really appreciate you and I know other folks will as well, so thank you.
Tony [00:13:29]:
And with that, folks just want to tell you guys about a very quick way that you can help support this show if you so choose, and then we'll jump right into the episode.
Tony [00:13:39]:
Another way you can help support the Spun Today podcast and also upgrade that stale wardrobe of yours is by going to spun today.com support and clicking on the banner for Stitch Fix. Once you do, you'll enjoy a $25 discount to your first purchase. And the way stitch Fix works is pretty cool. I use it and I've never been disappointed.
Tony [00:14:00]:
You'll set up a profile.
Tony [00:14:01]:
You'll put in all the sizes for your clothes, as well as all the different brands and types of clothes that you like to wear. It's really simple and intuitive to set up. They'll show you pictures and pretty much give you a thumbs up or thumbs down option on if you would wear something or not. And you get to select all the brands that you already are used to wearing. With this information, their thousands of passionate, trend setting stylists will curate a stitch fix box for you. They'll send you five items that you get to preview before they mail it to you, and you'll get to select based on the image if you like it or not. If not, they'll replace it with something else, and if so, they'll mail it to you absolutely for free. You can try everything on and you have a few days to send everything back or keep the stuff that you want to keep, then you can use that $25 credit that I mentioned towards your purchase of those items again to freshen up your wardrobe and also support the sponsorday podcast.
Tony [00:14:54]:
Go to spun today.com support and click on my affiliate link banner for Stitch Fix and enjoy your $25 credit.
Tony [00:15:05]:
All right, babe, so this year was a rough one for us and for the family and especially for you from the very beginning of the year, which I wanted you to help me clarify because I remember it being around Christmas time or New Year's, but definitely around that area. You were diagnosed with breast cancer. Thankfully it was detected early and we are going to get into how a bit later. Currently, as of the recording of this episode, you are two sessions away from finishing your chemo treatments and we definitely gonna get into all that stuff. But first, I wanted to thank you for coming on once again. And also I wanted to have this conversation because I think it's important for a couple reasons. One, for other folks that may be going through a similar situation to gain knowledge or from your experiences and just generally like strength and hope on like how to get through and that there is a light at the end of the tunnel which I think we both see now and also gain the knowledge of the gene test that detected this to begin with. Which again, we're going to speak about.
Tony [00:16:17]:
And I don't want to say most importantly or equally as importantly for our kids when they're old enough to really understand what's going on, I want them to have this to listen back on and just know what their mom went through and what a hero you've been throughout this whole thing. Cause you really have been.
Zoila [00:16:36]:
Thank you.
Tony [00:16:38]:
So thanks for coming on the sponsor day podcast.
Zoila [00:16:40]:
Thank you for having me. I feel so special.
Tony [00:16:46]:
Yeah, it feels like the dominican Joe Rogan experience.
Zoila [00:16:50]:
I know.
Tony [00:16:50]:
So, yeah. So Philadelphia, where it's gotten fuzzy for me, if you remember. I remember it being around Christmas time. Yeah, it was Christmas time when you were initially diagnosed. But let's go actually, let's go back a step to like, everything really started when you were thinking about doing the hysterectomy, right?
Zoila [00:17:10]:
So we had decided, well, I had decided that I wanted to have the surgery to not have children because we had decided two was enough, which is.
Tony [00:17:22]:
Definitely, definitely a good cut off for me because I know even way back you always kind of wanted more like three or four.
Tony [00:17:30]:
I wanted one or two.
Zoila [00:17:31]:
I wanted three. Not three or four.
Tony [00:17:33]:
I wanted one or two. But then after actually having the two kids, I think you kind of, like, walked back the three to two, maybe three.
Zoila [00:17:41]:
Even now I still want another one, but, you know, the situation is so. Well, thankfully, I decided not to.
Tony [00:17:49]:
Yeah.
Zoila [00:17:50]:
Cause that would have been a problem. The future.
Tony [00:17:53]:
Yeah, true, because nothing would have been detected. All right, so let's go back. So you decide to get the surgery to not have kids anymore.
Zoila [00:18:00]:
So I went to gynecologist, and they referred me to somebody to have the surgery done. I forgot her name. Doctor Sho. She was really great. So I went to see her at.
Tony [00:18:17]:
NYU Langone, by the way, which. NyU Langone, which is where both our kids were born. And they have been absolutely amazing. Like, with every single procedure, everything that you've had done, which we're gonna touch on throughout this episode, and they've been absolutely awesome. All the doctors, the staff, the facilities itself. Definitely high praises.
Zoila [00:18:37]:
Yeah. So I went for a visit just to speak about it and to see what my plans were and when I could have it done. And during the consultation, she said to. Since I had a history of cancer, of family history, would you add on.
Tony [00:18:56]:
Your mother's side, who had ovarian cancer?
Zoila [00:18:59]:
My mother had ovarian cancer. My grandmother. My maternal grandmother had breast cancer, and my maternal aunt also had breast cancer. So it was an extensive family line, you know, and my mother's side that had cancer or had, you know, passed in regards to cancer. So I had. She recommended to do the BRCA test.
Tony [00:19:33]:
Which is the gene.
Zoila [00:19:35]:
Yeah, it, like, tests you for if you have a mutation in the gene and if you're prone to have cancer.
Tony [00:19:44]:
Right.
Zoila [00:19:46]:
And I had done it before, but it was ten years ago, and I was negative then, but she recommended me to do it again just because she didn't have the results. And I didn't have it either, since it was in Massachusetts and I no longer have the information of my doctors or anything. So I was like, sure, I'll do it again, just so she could have the results. But I was, you know, carefree because.
Tony [00:20:14]:
I was negative before.
Zoila [00:20:15]:
Yeah, before. So I was like, okay, let's just do it.
Tony [00:20:18]:
And we didn't even know to factor in. But an interesting point is that the, like, at least for me, the way I thought about, like, genes, it's like, the genes that you have, other genes that you have. That's it. Which might be the case. I'm not a doctor or scientist or whatever, but the tools and the technology to detect change and evolve over time. So even though you were negative back then. The technology and, you know, gene identifying, you know, tests that they have now are more sophisticated and able to detect more, which they weren't before. And then that's why it.
Tony [00:20:58]:
If you want to continue with the results that you got from that.
Zoila [00:21:01]:
So it was negative back then. So I was like, oh, thank God. Back then. I was like, thank God it's negative. The thing is, if you are positive in the BRCA gene test, you have to make a decision, because that means that you have a percentage, a higher percentage of getting cancer and dying from it if it's a high percentage. So. And they specify what type of cancer.
Tony [00:21:28]:
It's usually, like, breast. Right? Breast or ovarian and or pancreatic.
Zoila [00:21:32]:
Pancreatic cancer. So I was negative for all of the back then. So I did the. It's a blood test, and they ask you questions like, what was the age that each of the family members died and when were they diagnosed with the cancer? So I filled that out, and I did the blood work, and they told me it would take, like, two weeks. I scheduled the. I forgot the name of the surgery. When you don't want to have a.
Tony [00:22:07]:
Kids, it was like the tube tying or the fallopian something. It wasn't like the full hysterectomy, right?
Zoila [00:22:14]:
No, no. I mean, they don't do full hysterectomy unless you have to. They always, you know, push that off.
Tony [00:22:21]:
Okay.
Zoila [00:22:22]:
Unless it's necessary.
Tony [00:22:23]:
But it was like one of the other one. Cause I know there's. They could, like, burn off the ovaries or tie the fallopian tubes or now they.
Zoila [00:22:32]:
They just burn it or cut it off.
Tony [00:22:34]:
It was like one of those that you had scheduled.
Zoila [00:22:35]:
They don't tie tubes anymore. They don't do that.
Tony [00:22:39]:
Okay.
Zoila [00:22:39]:
Because it wasn't really effective. Effective. And they could just untie themselves, I guess.
Tony [00:22:45]:
Mm hmm.
Zoila [00:22:47]:
And you're, like, fully sterilized. Sterilized that you call. No, well, whatever. That you.
Tony [00:22:55]:
You're fixed.
Zoila [00:22:55]:
I don't have any more kids. Yeah, you're fixed. So that was the case.
Tony [00:23:01]:
So you had made the appointment for that while you were still waiting on the surgery?
Zoila [00:23:03]:
I hadn't made the appointment yet for. To have the surgery done. And, like, midway, the doctor called me with the results. She did tell me that I was positive for the BRCA gene one. And she sent me over the results. So she said, unfortunately, you have to cancel the surgery, and now you have to make a decision what you're going to do if you're going to remove the ovaries. That was one option. Just remove the ovaries.
Tony [00:23:35]:
It was just the bRCA one or bRCA one and two?
Zoila [00:23:38]:
No, it was only one. The BRCA one. The BRCA two. I don't know what it is. I really didn't look into it. But it's another type of gene.
Tony [00:23:49]:
Based on the, like, the BRCA one results. The. Our understanding is that the likelihood of getting a type of cancer, and I think they give you percentages, is a lot higher. So then because of those results, you have the ability to do preventative surgeries or treatments and so forth, in general.
Zoila [00:24:18]:
Yeah. So I waited for the results to arrive in the mail. And the ovarian cancer, the percentage of me getting that type of cancer was 60%, which is huge. Yeah. And for breast cancer, was 40%, which is also huge. It is very big.
Tony [00:24:42]:
You have, like, a coin flip of a chance of getting either and even more, which is scary as shit. I remember.
Zoila [00:24:51]:
I mean, it was scary because I knew that I had to make the decision, like, what I'm gonna do, because.
Tony [00:24:57]:
Then it changes the plans for, like, the procedures that you already had scheduled to have. Because now it's not just about, you know, not having children anymore, it's about not getting cancer. Not getting cancer, yeah, exactly. So then that changed the. That plan of, like, the surgery, the type of surgery that you're gonna have there. Right.
Zoila [00:25:19]:
Well, it made it easy for me because I wanted to have the hysterectomy anyways, but I wasn't approved for it because they don't approve you unless it's a. There's a reason for.
Tony [00:25:30]:
Medical reason.
Zoila [00:25:32]:
But I was like, whatever, I'm gonna take out my ovaries. So why would I stay with my uterus and get my period every month?
Tony [00:25:40]:
Still dealing with that silver, silver lining up for nothing. No periods.
Zoila [00:25:44]:
I was like, really? And I still have to deal with periods even though I don't need it anymore, just because of the hormones or whatever, you know?
Tony [00:25:54]:
Yeah.
Zoila [00:25:55]:
It was so annoying. Well, women, we understand. We don't want no more periods. It was pointless.
Tony [00:26:03]:
So that was kind of a plus. So, yeah, it kind of made that decision a little easier because of the fact that you already were down to not have kids anymore. So this cancer scare of, you know, somebody telling you, hey, if you don't do something, there's a 60% chance that you're gonna get ovarian cancer, but if.
Zoila [00:26:19]:
You remove, you have a total hysterectomy.
Tony [00:26:21]:
A total hysterectomy. Remove everything.
Zoila [00:26:23]:
Very low percentage.
Tony [00:26:25]:
It's like a minimal, like 4% chance or something like that. I think I remember.
Zoila [00:26:30]:
But it's like the lining of your.
Tony [00:26:32]:
It's like the lining of the uterus or uterus or like that area.
Zoila [00:26:36]:
Like, they can't say 100% exactly, because they can't.
Tony [00:26:40]:
So it goes from 60 to four, which is, you know, a no brainer in that case.
Zoila [00:26:46]:
The only bad thing, if I did have a hysterectomy, I will go into menopause full blown, and I still haven't received any bad symptoms yet. But because I'm on hormone patches, right. So I regulate the symptoms.
Tony [00:27:05]:
Right. So, like, the hormone patches kind of replace. I guess my rudimentary understanding is that it replaces or tries to supplement for the hormones that your uterus is not and ovaries are not producing anymore. And that wards off, like, the menopause. Heat, hot flashes and stuff.
Zoila [00:27:23]:
Night sweats. Yeah.
Tony [00:27:24]:
All that fun stuff.
Zoila [00:27:26]:
No more sexual urges and stuff like that. So it's a lot of things that we don't know unless we're in that world. And I found out, like, okay, so I'm gonna go into menopause. I was like, okay, that's fine. It's not a big deal, but until you're in there, you don't know what's going on.
Tony [00:27:48]:
Exactly. All right, so then you did the hysterectomy.
Zoila [00:27:53]:
So then I decided then we had, like, a telehealth with a surgeon, and she explained, like, I could take out the uterus and the ovaries, or I could just take out the ovaries. And what the plus and the minuses was both things.
Tony [00:28:13]:
There was one scenario where you take off. I forget which one, and it still produces estrogen or progesterone or something like that. So then you don't have to get on the patch, but then if you take everything out, you get on the patch, the hormone patch, which increases the risk of getting breast cancer. It's like a weird thing.
Zoila [00:28:33]:
You get one thing, and then it increases the chances for you to get breast cancer anyway.
Tony [00:28:38]:
Right, exactly.
Zoila [00:28:39]:
So, like, we were like, let's just take everything out. And that's what I wanted in the beginning anyways. It's just that now I have a reason, you know? Like, why risk it?
Tony [00:28:51]:
Yeah.
Zoila [00:28:51]:
It made it better to have it less liable to have cancer.
Tony [00:28:55]:
Right.
Zoila [00:28:56]:
At all.
Tony [00:28:56]:
It made a much more clear decision.
Zoila [00:28:58]:
Mm hmm. So then I scheduled the hysterectomy, and that was the first surgery I had ever done. I've never been on a surgery beside.
Tony [00:29:09]:
Well, yeah, the childbirth and stuff like that, but that's not really.
Zoila [00:29:12]:
Oh, that's not surgery.
Tony [00:29:13]:
Yeah, true.
Zoila [00:29:14]:
It's not like you got.
Tony [00:29:15]:
Yeah, I'm thinking, like, medical procedure, but, yeah, you're right. So it's scary.
Zoila [00:29:21]:
I was nervous. Yeah. Cause you don't know what you're gonna feel. You don't know if you're gonna feel anything. Well, it should. That's the fear that you're gonna feel.
Tony [00:29:28]:
That you're gonna wake up in the middle of it.
Zoila [00:29:30]:
You're gonna wake up in the middle of the surgery, or you're gonna feel something. You don't know how you're gonna recover. You don't know what you're gonna feel afterwards. Those are like, the fears.
Tony [00:29:40]:
Yeah. The scary surgery. Unknown.
Zoila [00:29:42]:
Yeah, well, you don't know. So then I scheduled it. The surgery after I cried, like, after the doctor told me all the results. In the beginning, I did cry. I didn't. Like, she was like, I'm so sorry. And I didn't understand. Like, I hadn't grasped that.
Zoila [00:30:02]:
That means that you have to decide if you're gonna get a hysterectomy, which wasn't a, you know, like, a big thing. But she, as a doctor, knows that it is a big thing.
Tony [00:30:12]:
Yeah.
Zoila [00:30:13]:
Especially, like, if you haven't had kids or anything. Like, for me, in that point, I already had my kids, but she's like, what if it's a big deal for you, you know?
Tony [00:30:25]:
Yeah, right, right.
Zoila [00:30:27]:
So she doesn't know my situation or whatever.
Tony [00:30:29]:
Yeah, true.
Zoila [00:30:30]:
And then I was like, oh, man. So now I have to decide what I'm gonna do. And also, since I was gonna be on the hormone patch to not get symptoms for the menopause, it increases the chance, the chances of breast cancer with the hormone patch. So that was a big thing, too.
Tony [00:30:49]:
Because you're already at 40% risk based on, like, the genes and tests.
Zoila [00:30:54]:
Yeah.
Tony [00:30:55]:
And then the patches could increase that.
Zoila [00:30:57]:
Exactly. And it does say on the patches, like, your increased risk of risk of breast cancer. Okay, great. It's like you're curing one thing to get another.
Tony [00:31:11]:
It's like you're playing whack a mole with fucking cancer.
Zoila [00:31:15]:
Yeah, it's like scary stuff.
Tony [00:31:18]:
So after. After you did do the surgery, how'd you. How did it feel, that first surgery, the hysterectomy?
Zoila [00:31:24]:
I was. I didn't feel any pain. That was the best nap. It's like you. They. You have to walk to the surgery table and they tell you to lie down and they tell you like take deep breaths. You know, take deep breaths. And I'm like breathing and I'm looking at the light like that light in Grey's anatomy and all those shows or.
Zoila [00:31:47]:
And the dentist, you know, that big light. Yeah, they have that. It's a huge light in front of you and they tell you to take deep breaths and they gonna give. They were gonna give me something to calm me down and that's all. Like after that I. I woke up.
Tony [00:32:03]:
Then you got that Michael Jackson Napdev.
Zoila [00:32:05]:
Yeah, and then I woke up and you were there and telling me that it took like 3 hours.
Tony [00:32:11]:
Right, I remember, but it was. It was a minute. Yeah.
Zoila [00:32:14]:
And I couldn't, I couldn't like I saw blurry and that. I have like the hugest urge to pee. Oh, yeah, I remember that was like the thing. But I didn't feel any pain like in the surgery site or whatever, you know, I didn't feel anything. It felt like nothing. Like I had nothing done. But I had to pee a lot and I had to get up and go pee.
Tony [00:32:43]:
And you were kind of like sore and stuff, so I wasn't sore.
Zoila [00:32:47]:
It's just, you know, like when you're laying down for a long time and then getting up again, it's like you gotta take your time, like getting up. But it wasn't that like I had pain or anything.
Tony [00:32:58]:
And I remember they actually came, they had to measure your bladder with like a sonogram thing, machine or something to see how much you're emptying and if you're emptying your bladder completely and stuff like that. They did that a few times and. Yeah, I do remember that.
Tony [00:33:13]:
I forgot about that.
Zoila [00:33:14]:
I also had a sling.
Tony [00:33:16]:
Yes.
Zoila [00:33:18]:
Added because of my Ms. Cause I also have Ms, which, by.
Tony [00:33:24]:
The way, we did an episode about years ago when Soyla broke down, having Ms, being diagnosed with MS, living with it.
Zoila [00:33:31]:
Let's add another.
Tony [00:33:32]:
And it was. Yeah, it was. That's why I always say you're the strongest girl I know. All the shit that you've been through and continue to go through gracefully. But for folks interested, I will link to that episode, that specific episode related to MS, which is multiple sclerosis. In the episode notes, if anybody wants to go ahead and check it out. But because you had Ms, you decided to get the sling pee thing because it helps with.
Zoila [00:33:56]:
Yeah. And my bladder with not.
Tony [00:33:58]:
Not having to pee all the time.
Zoila [00:34:00]:
Oh my God. Because I always had like an urge to pee. Incontinence. I had incontinence so when I went to see the doctor that was gonna do the surgery for the hysterectomy, I told her that if it's okay if I wore a pad, because, you know, I had incontinence. So every little thing made me pee.
Tony [00:34:23]:
Mm hmm.
Zoila [00:34:24]:
Like, I used to leak, by the way. In other words, I used to leak. So she said, I'm just gonna refer you to a urologist. Just go see them, and they could do the sling at the sling.
Tony [00:34:40]:
That they could refer you to a urologist to get the sling. Yeah.
Zoila [00:34:43]:
The surgeon, she said, I could refer you to the, like, a urologist, and they could just do the surgery at the sling. On the day of the surgery of the hysterectomy. And I went for one visit, she said, you know, cough to see if you leak for a row. And I did. It was always an issue. I always had the urgency to pee, and I couldn't hold my urine that long. It's like a symptom from miss. And it had gotten better.
Zoila [00:35:14]:
Like, after I had my second child, it got way better, but it was still a problem, you know? And so I had it done on the day of the hysterectomy, too, and it really did help because they were.
Tony [00:35:30]:
Pretty much like, bama porochai that we're in there already. We could just, while doing the hysterectomy, the other urologist can come in, put the sling in, you know, whatever.
Zoila [00:35:39]:
And I was gonna be under anyway, so might as well kill two birds. Yeah. That time to do that.
Tony [00:35:45]:
Yeah.
Zoila [00:35:46]:
So I believe that's why I felt, like, the urgency to pee. But I'm not sure. Maybe it's just because of the surgery.
Tony [00:35:53]:
Yeah, probably just, like, general soreness and inside, you know?
Zoila [00:35:57]:
But, like, after the surgery, I had to pee, like, every 2 seconds. Like, every 2 seconds. Like, I used to go to the bed. I used to pee, go to the bed. And then, like, a minute later, I had to call the nurse. The nurse take me back, and they measure the pee. And then I used to go back to the bed, and I had to. I was like, oh, my God, I feel so bad for the nurse.
Zoila [00:36:23]:
And then she had to come, like, every 2 seconds.
Tony [00:36:25]:
And they even give you a bedpan, I think.
Zoila [00:36:28]:
No, they didn't give me anything. I had to go to the bathroom, and it was, like, so annoying. I spent the whole night like that.
Tony [00:36:35]:
Yeah.
Zoila [00:36:36]:
And then they. With a sonogram uterus thing, like a bladder monitor.
Tony [00:36:44]:
Bladder scan thing.
Zoila [00:36:45]:
Yeah. They used to see if it was empty or not. And, you know, eventually I got okay, but I stayed overnight that night.
Tony [00:36:54]:
Yeah, yeah.
Zoila [00:36:55]:
So they could test my bladder.
Tony [00:36:58]:
And then next day you're out and came home.
Zoila [00:37:03]:
Then recovery was really good. I felt like sometimes I used to feel pain. I used to take Tylenol, and I didn't want to take no opiates. It was more of that because I was, you know, I've seen so many documentaries.
Tony [00:37:19]:
We had recently watched dopesick and, like, that other.
Zoila [00:37:23]:
I know. So I was like, no, no, no. I don't want my life to change that way. It's okay. Like, I'll take tylenol and ibuprofen or whatever. They gave me, like, a muscle relaxer.
Tony [00:37:35]:
Yeah.
Zoila [00:37:36]:
And I recover pretty well. I didn't feel any pain, nothing severe.
Tony [00:37:42]:
And then. So when was that? That was, like, in the July. July of last year.
Zoila [00:37:47]:
Last year.
Tony [00:37:49]:
So then fast forward. The next thing that happens is either.
Zoila [00:37:55]:
So after the. The hysterectomy, I was seeing an oncologist because of the breast cancer gene.
Tony [00:38:04]:
Right. Which is the BRCA one that we mentioned earlier.
Zoila [00:38:07]:
Yeah. So I had to, like, constantly, like, every three months, go see the oncologist, um, just so she could monitor my breast and do the, like, the touch breast test and also, like, schedule the mammograms, the ultrasounds and the mrIs.
Tony [00:38:29]:
Right. Because they said that they would interchange. One. One time you do a mammogram, three or six months later, you do the MRI, then the mammogram, then MRI like that. Something like that.
Zoila [00:38:40]:
To always monitor my breast and that. To make sure there's nothing weird going on.
Tony [00:38:46]:
Right. Because of the higher percentage of breast cancer risk.
Zoila [00:38:51]:
So that's pretty much what I was doing since July, when I had the surgery until December.
Tony [00:38:59]:
And you did a mammogram and it was fine.
Zoila [00:39:02]:
I did the mammogram, ultrasound. It was fine.
Tony [00:39:05]:
Then the next visit, the six months later, or whatever it was, was the three months. It was every three months was the MRI.
Zoila [00:39:14]:
Then I had the MRI scheduled. Yeah. And I went for the MRI, and.
Tony [00:39:19]:
That'S where they picked up. That's when they picked up the mammal. And the sonogram did not pick up. And that brings us to around Christmas time. And then they send you for the biopsy.
Zoila [00:39:30]:
Yeah.
Tony [00:39:30]:
Right.
Zoila [00:39:31]:
They said that they saw something really small. I went back, like, for. After the MRI, I went back for ultrasound, that they go specifically to the.
Tony [00:39:39]:
Spot where they got a targeted area.
Zoila [00:39:42]:
And they told me they saw something really small, but I should have a.
Tony [00:39:45]:
Biopsy done to the area, and that's around Christmas time. So then we go to get the biopsy. Yeah, I remember that day in like four sales.
Zoila [00:39:55]:
And then biopsy is one thing as a whole, you know, other ballgame that.
Tony [00:40:02]:
Was like a painful thing.
Zoila [00:40:04]:
It wasn't painful. I think I was more scared than it was really painful because they do numb you in the area, but, like, it's like a machine that's. With pressure. It's like. I don't know, it's like a needle and they like, let it go and it hits you like it's like a puncture. They puncture the area or the. Whatever it is. And they do it like five times.
Tony [00:40:34]:
That's how they let go.
Zoila [00:40:36]:
Pop.
Tony [00:40:36]:
That's how they pull back the tissue or something to test.
Zoila [00:40:39]:
Yeah. And it wasn't painful or anything, but.
Tony [00:40:43]:
It was like a weird sensation.
Zoila [00:40:44]:
Yeah, it was a little painful afterwards, but I just put ice and it was okay. Yeah, but I think the nerves, like, not knowing what. What it was gonna be like.
Tony [00:40:56]:
Right. That definitely adds to it. Like, okay.
Zoila [00:40:59]:
Yeah, like, you don't know anything. Like, okay.
Tony [00:41:02]:
Plus the whole, is this cancerous or not at that point. And we were. It was around the holiday, so people were off. I remember it being literally right, like a day or two before New Year's. I think it was between New Year's and Christmas, like, around that time, like having to wait. Yeah. So we had to wait even extra for the results. Cuz, you know, it was a holiday.
Tony [00:41:22]:
It was a holiday. People weren't working. And then we get the results.
Zoila [00:41:30]:
We have to go in, right?
Tony [00:41:32]:
We.
Tony [00:41:32]:
I think we got the results. We read it.
Zoila [00:41:34]:
Yeah, we got the results. We have my chart and. And we read it, but we didn't understand.
Tony [00:41:39]:
Yeah, we didn't. It was in the, you know, medical jargon.
Zoila [00:41:43]:
So we started googling, which is googling, which we didn't get any answers anyways.
Tony [00:41:49]:
I don't. We didn't get any clear answers, but it did seem like it was cancerous.
Zoila [00:41:53]:
Mm hmm.
Tony [00:41:54]:
Which was scary, obviously.
Zoila [00:41:56]:
And we had to wait until the holidays were over. And I kept on messaging the oncologist, like, oh, can you just call me? Just tell me the result. Cause I can't wait until, like, the following week or whatever.
Tony [00:42:13]:
Yeah, until.
Zoila [00:42:14]:
But she was like, no, I want to see you. I was like, okay, that's not a good sign.
Tony [00:42:19]:
Yeah. So then we go in and.
Zoila [00:42:22]:
Oh, and the radiologist called us, the one that did the. And she did that.
Tony [00:42:26]:
Did the biopsy.
Zoila [00:42:27]:
Yeah, she called like the day after. And she did tell us that, you know, that they did see something and it does seem cancerous, but like, they don't know specifically, like at what stage or what we could do, like what type of treatment. They don't have the details. So I did know afterwards and to.
Tony [00:42:47]:
Speak to your oncologist and stuff like that and follow like the usual protocol.
Zoila [00:42:52]:
So then I had the appointment with the oncologist and she did tell me that I had breast cancer. Type negative, stage no, stage one a.
Tony [00:43:04]:
Stage one a, which is the, like, smallest, you know, the one a, if I remember correctly. It's like inside. It's referring to the sides of it. So it's like one 2 is considered one a or something like that. And I'll try to find something to link to the episode notes, if anybody's interested.
Zoila [00:43:26]:
Triple negative.
Tony [00:43:27]:
And it was triple negative, which is an aggressive type of breast cancer, which basically means that it's triple negative to hormones, like the three hormones, which plays into what types of treatment they can give you. Because if it was positive for estrogen or whatever, one of the hormones, they could give you some sort of cancer drug that's, you don't know, estrogen induced or something, or attaches to it somehow. Like, I have no idea how that, like, mechanism works. But basically, because it's triple negative, that means no other medications except for chemo they explained would be feasible, would be the only option. And then also making the decision of surgery if removing one side, moving both, like what you wanted to do, you're already at this increased risk. It's triple negative. We caught it early, thankfully, which they said was, was best case scenario. But you did have to make that decision, right, of what you wanted to do in terms of surgery.
Zoila [00:44:35]:
Both. Yeah, both breasts or just one where the cancer was.
Tony [00:44:40]:
Right.
Zoila [00:44:41]:
And she said you could just remove the breast with the cancer, but there's a possibility that you could get it on the other breast.
Tony [00:44:51]:
And then we be right back to the same situation.
Zoila [00:44:53]:
That's a no brainer. Why. And I'm gonna go through the surgery anyway, so I might as well just do it. Just do it. And I was like, oh, can I keep my nipples? The chances too, right? To keep the nipples.
Tony [00:45:11]:
And the, and that's, that's the plastic surgeon. So we're still at the, like, oncologist.
Zoila [00:45:17]:
Yeah, there was an oncologist too.
Tony [00:45:19]:
Okay, okay. I don't remember that part.
Zoila [00:45:21]:
Oh, no, no, no. It was the plastic surgeon. Yeah, yeah. But we had the, the appointment when, when I got the diagnosis. Then I had to see the plastic surgeon. Surgeon that was gonna do the surgery, and the plastic surgeon, which was gonna.
Tony [00:45:37]:
Do the, like, two separate appointments.
Zoila [00:45:39]:
So there was one doctor that does the mastectomy, and the other one does, like, the reconstruction.
Tony [00:45:46]:
Right, right. So obviously scary news, but so many things.
Zoila [00:45:51]:
Like, okay, you have cancer. Yeah. Okay. And you. You could remove one, or you could remove both breasts, or you could keep your nipples, but your increased chance that you're gonna get the cancer back.
Tony [00:46:07]:
Right.
Zoila [00:46:08]:
So it's, like, so many decisions to make.
Tony [00:46:11]:
Right.
Zoila [00:46:11]:
Right there.
Tony [00:46:13]:
Obviously, life changing decisions, either. Which way do you decide to go with it?
Zoila [00:46:17]:
Which is easy. Like, do you wanna get cancer or do you not wanna get cancer?
Tony [00:46:23]:
That, in a weird way, helps simplify, like, all those decisions. It's like, increase the chances of me not getting cancer and developing cancer. What I wanted to say, before I forget is that some women choose, famously, Angelina Jolie did this. Choose to get a mastectomy when they test positive for that BRCA one gene, even if they have not developed breast cancer, which is.
Zoila [00:46:47]:
Thank you for bringing that up, because I was gonna have the mastectomy done, but I was. Wait. I was contemplating doing it when my son was out of school in the summer. So they told me that I had to keep doing mris and mammograms and ultrasounds every three months to monitor my breast and to see that there was nothing weird going on. So I only did it once, the mammogram and the MRI and that before I got. My God.
Tony [00:47:21]:
Yeah, that's true.
Zoila [00:47:22]:
I was eventually gonna do the double mastectomy just to prevent.
Tony [00:47:26]:
To prevent it, but that this sped up the time.
Zoila [00:47:29]:
Allow me to get to that point.
Tony [00:47:32]:
So tell me, how was the mastectomy surgery to you, and how was it different from the hysterectomy after you made the decision to. In terms of, like, pain? Actually, before you tell me that, I'm remembering the. This surgery for the mastectomy was also kind of like a two in one. So after, like you said, we met the oncologist, met the surgeon, then we go to the plastic surgeon, which is going to focus on the reconstruction after everything, after the fact. And they all tell us a bit about their pieces of the procedure. But with the mastectomy, it was, you know, main goal to get the cancer out, which I remember, you know, waiting in the waiting room, because that's like, they also test the lymph nodes there to see if there's, like, any spread to the cancer at all. And it's where we would find out if obviously, like, I've heard horror stories from back in the day. I was actually recently speaking to my mom when one of my uncles.
Tony [00:48:29]:
Yeah, one of my uncles on my dad's side when he had surgery for cancer. This was when I was a little kid. So years ago, he came here from doctor. He got. He got operated on. He went back then he had to come back and get it, like another surgery. And then when they opened him up to do the surgery, they see there that it's spread everywhere and there's nothing they can do, which is crazy. That that's how I guess maybe technology differences, that's how they were able to detect.
Tony [00:48:55]:
But whatever that was always. That was like part of a fear in me that, you know, they realized something that they couldn't pick up with the testing and stuff like that. So while I'm waiting in the waiting room. So it's really like an Olivia when. After the surgery, I get the call, everything went well. And then, actually, I bumped into the doctor when she was leaving, and she tells me that everything went well. She didn't see anything weird. They got everything out, and I.
Tony [00:49:20]:
So no worries there. And that you were doing good and stuff like that.
Zoila [00:49:23]:
Yeah. The day after. The day before the surgery, I had to go into the hospital. They had to inject a liquid into my nipple.
Tony [00:49:35]:
Oh, shit. Yeah.
Zoila [00:49:36]:
So they could. The day of the surgery, it's like a luminous type, a radioactive type of liquidity that. The day of the surgery, they put another liquid in after I'm under. So it depends. It, like, tells you which lymph node they have to remove by that liquid. It's like the weirdest thing, but it's nuts. That was like a whole nother thing.
Tony [00:50:04]:
Yeah.
Zoila [00:50:05]:
I was scared. It didn't hurt at all. I think I was just scared of what it will feel. Like. The unknown always is always the thing. Because it was like my first surgery. Like, not my first surgery, but my first injection into my nipple. Like what? So I didn't know what I was gonna feel.
Zoila [00:50:25]:
It wasn't painful at all. I didn't feel anything. So that was one thing.
Tony [00:50:29]:
Yeah, that was like a side thing. That's a whole procedure in itself.
Zoila [00:50:34]:
So I survived that.
Tony [00:50:36]:
Then you have the mastectomy. We were already told that after, you know. So they remove everything. Then the plastic surgeon and her team come in and they put something in you called expanders, as well as drains, which are literally. It's exactly how it sounds. Like plastic tubes sticking out of her with, like, pumps, pump looking things at the end. You know what it looks like? It looks like when you go to the doctor and you do pressure cuff. The pressure cuff? Yeah, like the blood pressure test.
Tony [00:51:09]:
And they squeeze that little bulb. It's like that. It's like a tube sticking out of both her breasts that wrap around her breasts, and it's draining, like, liquid and blood from post surgery. And they put that as well as the expanders in you, because after the fact, then you come home and. Which was, I think this was like, a tougher recovery, definitely. Then. Then the hysterectomy, because part of it is draining those drainers, or whatever they're called. Draining them and then putting them into little cups to measure how many cc's and writing them down and doing that for a week.
Tony [00:51:49]:
It was supposed to be, but it took you, I think, like, two weeks because they want the. The fluid to go down or the amount of fluid that your body is expelling to go down enough to a certain point to take the drains out. And it took you a little longer than originally expected. Yeah, that was a whole. Whole thing. How did you feel, though, like, during that time, that transition from getting the mastectomy, getting the expanders put in, which the point of the expanders is, you know, they cut a lot of skin, they stitch everything up, tighten everything completely flat. Completely flat. That had to feel weird as a woman.
Zoila [00:52:25]:
I mean, it was weird when I saw it because it's like a new thing to see.
Tony [00:52:30]:
Used to seeing your body.
Zoila [00:52:31]:
Yeah. And I said bye to my.
Tony [00:52:33]:
Yeah, me too.
Zoila [00:52:36]:
Bye. I'm not gonna see you anymore. Yeah, and bye to my nipples, too.
Tony [00:52:41]:
Yeah.
Zoila [00:52:42]:
That's a whole nother thing. You know, you have to get used to the new.
Tony [00:52:47]:
Yeah. The new.
Zoila [00:52:48]:
New chapter, the new self. It wasn't, like, really painful. It wasn't that painful. I mean, I was very consistent in my medication, like, to. And stop taking it, but it wasn't really, like something that I couldn't take or stand.
Tony [00:53:06]:
Yeah.
Zoila [00:53:07]:
So it wasn't really that painful. I mean, it was uncomfortable to be with drains.
Tony [00:53:12]:
Yeah. Cause you couldn't shower fully.
Zoila [00:53:15]:
I had to take, like, you had to sit down. Four baths.
Tony [00:53:17]:
Yeah. I helped you shower stuff. Sponge baths. Yeah. Doing the drinking.
Zoila [00:53:24]:
You had to sit down during, like, baths and stuff like that. But it wasn't really, like, painful that I couldn't take.
Tony [00:53:32]:
Just more uncomfortable than anything else.
Zoila [00:53:34]:
Yeah.
Tony [00:53:35]:
And then the. So then eventually, after a couple weeks, the drains come out. We go for another visit. Drains come out. Which they literally just, like, pull them out. So you feel them sliding around your boob and coming out the tubes.
Zoila [00:53:48]:
They literally, like, just push it. And that feels really weird.
Tony [00:53:52]:
Yeah.
Zoila [00:53:53]:
And it's uncomfortable. It's not painful.
Tony [00:53:56]:
It's just like a weird sensation again.
Zoila [00:53:58]:
Yeah. You feel the tube sliding off, but you're numb. You're a little bit numb from the surgery, so. And you do feel a lot of numbness.
Tony [00:54:12]:
Yeah.
Zoila [00:54:12]:
Like, around the area around the breasts.
Tony [00:54:15]:
Yeah. Because part of the, you know, getting rid of the cancer is then removing.
Zoila [00:54:20]:
One of the symptoms, too. You feel, like, really numb.
Tony [00:54:23]:
Yeah, a lot. You have, like, some nerve endings around there and stuff like that. Cause if not, then your skin could die. But it's very minimal.
Zoila [00:54:31]:
And it's not minimal.
Tony [00:54:32]:
What do you mean?
Zoila [00:54:33]:
I. Like, I feel it around, like, my breast is numb. Like, my armpits are numb by the breasts on. Yeah. Like, and around my breast is numb?
Tony [00:54:43]:
Yeah.
Tony [00:54:44]:
Like, completely.
Tony [00:54:44]:
You don't feel nothing at all?
Zoila [00:54:45]:
Like, I feel a little bit, you know, like, very mild.
Tony [00:54:49]:
Yeah. Yeah.
Zoila [00:54:50]:
But you know what the most uncomfortable thing is? When you're itchy, like, you feel the itch, but when you scratch, it doesn't relieve.
Tony [00:55:00]:
Oh, it shouldn't, but you still feel.
Zoila [00:55:02]:
Itchy and you're, like, scratching. It's the weirdest thing.
Tony [00:55:06]:
That is weird.
Zoila [00:55:06]:
And it's very uncomfortable.
Tony [00:55:08]:
But that makes sense. It makes sense, but it is weird.
Zoila [00:55:11]:
Yeah.
Tony [00:55:12]:
So then they. So at the plastic surgeon, they remove the drains and they also do something with the purpose of the expanders that are there are to expand the skin, the skin tissue on the breast to the point where, you know, little by little, you have to go multiple times to multiple visits. You go in, they literally just inject you to expand them. Hence the name expanders. And the point is to expand your skin to the point of wherever you want it to be for when you get the reconstruction surgery.
Zoila [00:55:48]:
Yeah, when you get the implants.
Tony [00:55:49]:
The implants.
Zoila [00:55:50]:
I mean, there's a lot of options. You could just go flat if you want to. If you don't want to go through the surgeries or just go, like, small also. But I wanted, like a normal. Well, normal for me.
Tony [00:56:04]:
Yeah. Like where you were. Like, where I was before now. So this is after. After all the surgery, after the drains come out, then we have to go into the phase of chemotherapy, which is a whole thing in itself, obviously, every. Everybody who hears chemo, especially myself, it's like a scary thing.
Zoila [00:56:24]:
Imagine furby.
Tony [00:56:25]:
Yeah.
Zoila [00:56:26]:
I have to go through it.
Tony [00:56:28]:
That's what I want to ask you about how is it from. Because they gave us the plan from the beginning, right? Which is, you know, the mastectomy. Go see the plastic surgeon. You're gonna need twelve rounds of chemo as a, as a prevent, as a preventative measure. So like we knew the game plan, but to me, from my perspective, it's like, all right, let's get past the first goal. Then we'll, we'll look at the next thing, whatever the next thing is. Then we'll focus on that. Then we'll focus on that.
Tony [00:56:53]:
So now we're in the phase of focusing on chemo. That's how I just like in turn processed everything. How was it for you, as again, being the one, like you said, to actually have to go through all the surgeries and then the chemo. And how has that experience been now that you've had the ten sessions of the twelve sessions with chemo?
Zoila [00:57:13]:
Well, when we went to get the diagnosis, they did tell us that we have to, that I had to do twelve chemos. It's like two weeks and then one week off.
Tony [00:57:26]:
Two weeks on, one week off. So we'd go every week.
Zoila [00:57:29]:
So one week is of two medicines.
Tony [00:57:32]:
Two different types of chemo.
Zoila [00:57:33]:
Yeah. And the second week or the week after is one medicine, one of the.
Tony [00:57:40]:
Those same medicines, those same chemos.
Zoila [00:57:41]:
And then the following week is the best week because you have a week off.
Tony [00:57:45]:
Yeah.
Zoila [00:57:46]:
And then the best thing ever.
Tony [00:57:48]:
Right. And then the week after that, then you go back to the two chemos, then the week after that, the one. And it's like that until you finish the twelve sessions and the process itself. Well, actually, let me go back. So how did you feel knowing that you had to take chemo? And I guess like more emotionally, I feel like you would think about your mom who went through that and passed. How do you feel, you know, having to take that on?
Zoila [00:58:17]:
Well, I know you want me to tell you, like, oh my God, I felt like, like a whole thing, you know?
Tony [00:58:22]:
But tell me how you felt.
Zoila [00:58:23]:
Really? Like, I really didn't think about it that much. I think that's how I went through it. Like, okay, I'm just gonna do it. And the good thing is that I'm used to getting infusions, right? Because of the Ms. That's the treatment that I take. I take an infusion every six months. So that prepared me. Look, okay, I have to go to this thing every week instead of every six months to get an infusion.
Zoila [00:58:54]:
Like not thinking about it, I think that's how I went.
Tony [00:58:57]:
Right. Which is. Which is admirable in a way, because as me, which is why we balance each other out. Well, because I overthink. Right now, somewhere in the back of my mind, I know I have to wash the car, and I'm contemplating if after this, I'm gonna go wash the car and then get the kids or get the kids and take them to wash the car. And, like, depending on, like. And I'm, like, I, like, overthink every single thing. So it's.
Tony [00:59:20]:
It's. It's an interesting balance that we have that just why we. We work well together, I feel. But.
Zoila [00:59:28]:
And I don't overthink things at all. I don't. Like, I think that's the. The way I managed to get through things.
Tony [00:59:36]:
Mm hmm.
Zoila [00:59:37]:
Because if I pay mine to it, then I'll get depressed. And. And I like why myself in that.
Tony [00:59:45]:
Position, you know, that definitely wouldn't help, which would be normal and expected, even. So. Which is why it's even more.
Zoila [00:59:52]:
And with my mom, like, I really didn't go with her to get treatment or anything, so I didn't know, like.
Tony [01:00:00]:
What she went through with the child.
Zoila [01:00:01]:
What she went through. Like, I. What? Like, I saw her, like, going through it, like, afterwards, like, after the chemos that she used to go home and. And all that, but my mom also blocked that from. Blocked me from seeing all those things, so I really didn't know what she went through.
Tony [01:00:18]:
Right.
Zoila [01:00:19]:
So, in a way, that helped, too, because I didn't know anything.
Tony [01:00:23]:
It was still, like, unknown. And you felt prepared, like you said, because it was like, I get these infusions, which is literally an iv medication for mass every six months. Now I'm just gonna go get more infusions, a different type of medication. And you, like, used to, like, the. At least the process of it, the physical process of it. Before getting the chemo, though, something I just remembered was the port surgery. So for the chemo, you either had the option of, you know, getting. Getting the chemo in your arm, but they.
Tony [01:00:54]:
They recommended getting a port because you were gonna have so many sessions. And the chemo medication is strong and could, like, fuck with your veins and, like, really break it down and stuff. So a poor is literally, like, a device that they put into your chest.
Zoila [01:01:09]:
Area or your arm or your arm.
Tony [01:01:12]:
Okay. I didn't know they could do it in arm, but for you, they put it in the chest area, where you literally have, like, this device in there that's connected to the vein already. And then they seal you up aortic.
Zoila [01:01:24]:
Vein or something like that. So.
Tony [01:01:27]:
And which makes it easier to, like, you have that device in you this entire time. So every time we go to get the chemo, it's in the morning. First stop is blood work. Like, we wake up, like, at six something in the morning point, usually, like, around 737 45, get blood work, then go upstairs and see the doctor, the oncologist, discuss your blood work, how everything is looking, how you're feeling, and all that good stuff. And then from there, then go get the chemo, which they use that same port to give you the chemo medications from. And I remember the port surgery itself, the port surgery, which was another. Another side procedure thing. That definitely adds up.
Tony [01:02:15]:
It was an outpatient, same day thing. But when you went to get the first drawing of blood, it hurt like crazy. You got nauseous. You were almost gonna throw up.
Zoila [01:02:26]:
No, but let's talk about the surgery.
Tony [01:02:28]:
Or the surgery itself. Go ahead.
Zoila [01:02:29]:
Because the surgery was like the. Not the surgery itself, but recovery. It was really painful.
Tony [01:02:36]:
From the port?
Zoila [01:02:37]:
From the port. Because it's like you could feel it, like something strange in your body. And since I had the. I was uncomfortable with the expanders, because the expanders are not very comfortable either.
Tony [01:02:53]:
True. Like, your skin stretching, and you feel something hard.
Zoila [01:02:56]:
It feels like you have a rock, your chest. Chest, or a balloon. Something foreign inside your body, in your breast area, and it feels really strange. So you're adding something strange to your body again by adding a port. And the recovery was not easy. It was painful, and you had to use it for the chemo.
Tony [01:03:22]:
To be able to get the chemo. Yeah.
Zoila [01:03:23]:
So, like, it's recovering. Like a surgery is recovering, and you also have to use it.
Tony [01:03:29]:
Right.
Zoila [01:03:30]:
You know, so it's like, oh, my God.
Tony [01:03:32]:
Which made it even worse. And then we got some good tips from the doctor of nurse. The nurse. The nurse, too, to put, like, lidocaine on it at, like, the cream before going in, in the morning, so it could start numbing. And also eat something in the morning and take the nausea medication to.
Zoila [01:03:53]:
So the first time that I. That they inserted the, like, the catheter inside the port, it's like. Like a little square with a needle at the end, and they just have to insert. Insert that needle to the port, which is a round thing inside your. Your body. You don't see it, but it's there. So I felt like the first time that they did it, she's like, okay, I'm gonna count to three. Insert the port, and then count to three and put your chests out.
Zoila [01:04:26]:
And I was like, okay. She said, one, two, three. And I put my chest out, and that felt like I was being stabbed once. And I was like, oh, my God, like, how I'm gonna do this twelve times.
Tony [01:04:39]:
Yeah. How the heck I remember you telling me that?
Zoila [01:04:42]:
Because it was, like, the worst. It's like being stabbed. That's how I felt like being stabbed once. And, okay, go.
Tony [01:04:50]:
That's nuts.
Zoila [01:04:50]:
Go and get chemo.
Tony [01:04:52]:
And what, right on top of that, for your prize of getting stabbed, go get chemo. Which is crazy. Crazy, because out of the mastectomy, the hysterectomy, like those big surgeries, like the port surgeries, fucked with you the most in terms of, like, pain.
Zoila [01:05:07]:
And I thought I was gonna be okay with the port. I was like, okay.
Tony [01:05:10]:
I thought that was like a nothing. Okay, so then, now, oh, something we definitely have to speak about, which was news to both of us. Anybody else that I've mentioned it to had never heard of it before. So it's definitely a tip for anyone going through chemo if they want to, want to try this. But they told us, the oncologist told us about cold cap therapy, and what it is, essentially, is a helmet looking device that you put on, and it gets attached to a machine that pretty much freezes your scalp, freezes your head. Not literally frozen, although it feels, like, literally frozen to you, but it, you know, I don't know if it's hydrogen or whatever it is. It gets super, super, super cold. Like, ice cold turns to ice.
Tony [01:06:00]:
Literally, it feels like an ice pack, like one of those ice packs in the freezer, and it freezes your scalp. And the. The mechanism of how it works is that you're getting chemo. It's going through your blood. It's cycling through your body. And that's why a lot of people experience hair loss and go completely bald in a lot of cases, because the chemo is so potent and strong, when the blood is circulating through your scalp and through your body, it just kills the hair follicles, and it falls off. But with the cold cap therapy, it freezes your scalp to the point that the blood doesn't circulate there. So.
Tony [01:06:37]:
Or as much. So it's the blood with the chemo. So it minimizes the hair loss, which you have experienced hair loss and thinning. But if nobody knew you were going through chemo, nobody would even notice.
Zoila [01:06:51]:
No.
Tony [01:06:52]:
Like, it's been. And also, it helps that you have very, very, very thick.
Zoila [01:06:56]:
A lot of hair.
Tony [01:06:59]:
Hair, exactly. And, you know, that was just something that, you know, it elongates the whole process because you have to do the cold therapy depending on the chemos that you're getting for that day. But on the high level, you have to do half hour of the cold cap therapy before you even start the medication. And then after you finish the two chemos, if you're getting two that day, you have to do an hour and a half of the cold cap therapy afterwards as well. On top of everything.
Zoila [01:07:29]:
And during.
Tony [01:07:31]:
And during. Yeah, throughout the whole shit.
Zoila [01:07:33]:
Yeah. So I was like, I didn't think that I was gonna care. You know, I was like, it's okay. Like, it'll grow back.
Tony [01:07:42]:
Yeah.
Zoila [01:07:42]:
I think it's that same mentality. Like, no, don't think about it. Like, it's okay. It's not a big thing.
Tony [01:07:49]:
And I was more on the side of.
Zoila [01:07:51]:
But you were like, no, if there's a chance.
Tony [01:07:54]:
Yeah, because I'm thinking also from.
Zoila [01:07:57]:
But I'm thankful that you did say that because, like, okay, so I should care a little more. Like, you know, like, wake up.
Tony [01:08:06]:
And honestly, it has zero to do with my. My, you know, personal want or whatever, because I don't factor myself into that in this situation. But it was a twofold thing. I had a conversation with an old coworker of mine who had a girlfriend that went through breast cancer and chemo and stuff like that. And one of the things that stood out to me that he told me, shout out to dash is that one of the most traumatizing things of everything that his girl went through was losing her hair. And that he, as a guy, were like, you know, who gives a fuck? Like, whatever. So he was kind of like, why would that be, like, traumatizing? But he didn't think of it as a traumatizing thing until it happened. And then realizing when it happened, how much it affected her and she kind of had that attitude as you.
Tony [01:08:54]:
I would imagine that, you know, it is what it is that. And then also, I was thinking of the kids and them seeing you. I feel like if they saw you, you know, without the hair, which, you know, obviously it's no. Under nobody's control if they're gonna lose their hair or not.
Zoila [01:09:10]:
But if there's something that could prevent.
Tony [01:09:11]:
It, that it would be traumatizing for them. So if there's a chance that you could prevent it or minimize it, as in your case, then it's definitely worth the shot. Even. Even though it's not something that's covered by insurance. But it's.
Zoila [01:09:26]:
But they could help you financially if you apply for financial assistance.
Tony [01:09:30]:
Exactly. And it was like, even if you pay out of pocket, I think it was like two grand or something like that. 2424 hundred and you could apply for financial assistance.
Zoila [01:09:38]:
But it depends on the treatments that you have and the type of treatment that you're getting. So it all depends on that.
Tony [01:09:46]:
Right. But definitely cold cap therapy. I recommend it. And also, like, that icing thing. It sounds like a primitive thing, but seems to work for multiple things. Not just the. The cold cap, but also patients ice their hands and their feet because they get like, tingling and stuff. Right.
Tony [01:10:04]:
You've experienced that, like, on the hands that I think you said it felt like little ants. Like little ants.
Zoila [01:10:11]:
And it is painful.
Tony [01:10:13]:
I could imagine. Like, if you feel your skin crawling, it's super uncomfortable and you can't do anything about it. But with the ice, while you're icing it, less of the chemo goes towards your hands, you know, same type of mechanism, less of the chemo circulates through your hands.
Zoila [01:10:26]:
It's not a comfortable thing, but you have to do it, like, to feel better. Like the cold cap, it's. In the beginning, it didn't hurt because of my hair. It was fine. But then when your hair starts falling out and it gets bent, you do feel it a lot in your head. Like the first starting or 20 minutes of it. Like, you feel brain freeze. Like, full on brain freeze.
Zoila [01:10:51]:
Like, your eyes hurt, your head hurts. So I take Tylenol before I leave to the hospital. So that makes it better. But it's uncomfortable. And then your scalp goes numb because it's so cold, it just goes numb. And then you don't feel. And then you just, like, pressing to see if it's working. And it is.
Zoila [01:11:11]:
That's how Numa gets. Like, you don't feel it at all, but the first ten minutes, 20 minutes, it's not a good thing.
Tony [01:11:19]:
But definitely the cost, the benefits.
Zoila [01:11:23]:
It does work. Yeah, I do see, like, they. It does fall out. The hair does fall out. I mean, I've lost a lot of hair. But, like, the main part that you could cover the balding areas, at least you could cover that part with your hair.
Tony [01:11:41]:
Yeah.
Zoila [01:11:42]:
So, you know, like, the kids, they haven't seen anything scary yet. Yeah.
Tony [01:11:47]:
Yeah, definitely. And now that you are almost done, well, at least with this chemo phase of it, because then we'll be, like, officially, officially done once you have the reconstruction surgery. But how does it feel?
Zoila [01:11:59]:
But going back to the Portland, which made a lot of difference. Putting on the latocaine to numb the area before they entered the port or the catheter into the port, that did help a lot. So it's just a suggestion if you are going through it. I mean, some people don't feel pain when they get the catheter inside the port. So it all depends on the person. But I did feel pain. I felt the stabbing pain.
Tony [01:12:29]:
Worse than surgery. Yep.
Zoila [01:12:32]:
So. And I felt pain, like, recovering. It does get better. Like, now I don't feel it.
Tony [01:12:37]:
But you're still doing the lidocaine and all that stuff just as a preventative. Yeah. That's an important point. So to wrap things up, how do you. How does it feel to almost be done with chemo? To me, it feels, like, exciting. And to get to the end of that phase of it and especially not to have to see you going through that and just, like, the nausea and how shitty you feel afterwards, which is something we didn't mention, actually. How after?
Zoila [01:13:07]:
Well, after the chemos, when I get the two medicines, the two chemos, what I mainly feel is, like, nausea. And I have this horrible taste in my mouth. It's not a metal taste. It's, like, medicine. Like, full on medicine. Like, if you put a Tylenol in your tongue and you leave it there, like, that taste, and it's, like, triple that. It's like, it makes you more nauseous.
Tony [01:13:32]:
That taste, like, it exacerbates the nausea.
Zoila [01:13:35]:
And you can't taste food. Like, nothing is enjoyable. Food, water, drinks, everything is, like, blah, you know, like. And exhaustion. You feel really tired. Like, walking is hard. Everything is harder.
Tony [01:13:51]:
It feels like your body's just beating down.
Zoila [01:13:53]:
Yeah. I mean, you have a lot of medicine in you, and you feel it. You feel like you have a lot of medicine inside you. Like, oh, my God.
Tony [01:14:00]:
Yeah.
Zoila [01:14:02]:
How do I feel that? We're almost done? I'm very happy, and I'm very looking forward to the plastic surgery, the reconstruction. I guess that's what's pulling me through the whole thing. Like, okay, just get through this. Get through one more. Like, I've been counting. Okay, one more, one more, one more. Um, to get me through this. The silver lining is a reconstruction.
Tony [01:14:30]:
Yeah, absolutely.
Zoila [01:14:31]:
So that's the motivation and that I want to be done with this, too.
Tony [01:14:35]:
Yeah, absolutely. I couldn't agree more. And I'm very, very proud of you. And again, I'll say it again. I've told you before, I said it earlier. You're the strongest girl I know.
Zoila [01:14:45]:
The secret is not to think about. Don't think about it. Try it, try it. Maybe it helps you. You never know.
Tony [01:14:53]:
Yeah, absolutely. Well, folks, that was.
Zoila [01:15:00]:
I just hope that this helps somebody, you know, that's going through anything.
Tony [01:15:06]:
Absolutely. That was the hope for this episode. Hopefully somebody listens to it and learn something that they didn't know before or gains some, like we said in the beginning, some hope, some strength to get through whatever you're going through now. If it's something similar, and yeah, yeah, that's pretty much it. Thanks for listening, guys.
Zoila [01:15:25]:
Free Palestine, peace.
Tony [01:15:31]:
And that, folks, was episode 266 of the Spun Today podcast. Thank each and every one of you very much for listening. Thank you once again to my lovely wife, Zoila. Thanks for taking the time sharing your story. I'm sure folks will get a lot from it. And for everyone listening for links and different things referenced throughout this episode, as well as some photos, go to sponsoray.com podcast Forward Slash 266, which is the webpage for this specific episode, and please let us know what you think. Share your story within the comments, wherever it is that you're listening to this, and let's get a little community of support going around this. Thanks again for each and every one of you for listening.
Tony [01:16:12]:
I really appreciate it. Please stick around for a bit more to listen to. A few different ways you can help support this podcast if you so choose. Check you guys out next time. Peace.
Tony [01:16:24]:
What's up folks?
Tony [01:16:25]:
Tony here. I hope you're enjoying the Spun Today podcast as much as I enjoy producing it for you. Here are a few ways you can help support the show. You can support the Spun Today podcast financially by going to spuntoday.com support. There you will find a couple different ways that you can do just that, some of which will actually not even cost you a dime, such as using my Amazon affiliate link. When you go to sponsodate.com support, you'll see my affiliate link to Amazon. Click on it and it will take you to Amazon's website where you can do your shopping like normal. This will not cost you anything extra, but Amazon will pay me for driving traffic to their website.
Tony [01:17:06]:
If you'd like to support the podcast more directly, you can do so by becoming a Patron@spuntoday.com. support you'll also find my Patreon link. This is where creators such as myself can be paid directly by patrons like you. You can either make a one time donation or schedule recurring donations if you so choose. There are also different tiers of support, and depending on which you decide to go with. You'll also receive some perks in return, such as early access to content, free digital copies of my books, free bookmarks, etcetera. That is again, by supporting via my Patreon link available@sponsoday.com support similar to Patreon, at that same location you'll also find my ko fi link as well as my buy me a coffee link. They work very similar to Patreon and are different ways you can help support the show financially.
Tony [01:17:55]:
And last but certainly not least, you have the good old fashioned PayPal donation button. Any which way that you choose to support is greatly appreciated. It all helps me do more of what I love, which is writing and podcasting. Again, go to spuntoday.com support. You can also support the Spun today podcast by rating and reviewing the show. Wherever it is that you're listening to.
Tony [01:18:18]:
This episode, I'd really appreciate it because.
Tony [01:18:21]:
It really does help. Also, follow me on all socials on today on X, formally known as Twitter Puntoday, on Instagram, and today on YouTube, where you'll not only find full length episodes of the podcast, but also chopped up clips and additional content. And of course, you can follow the Facebook page@facebook.com spun today another way you can help support the Spun Today podcast and also upgrade that stale wardrobe of yours is by going to spuntoday.com support and clicking on the banner for Stitch fix. Once you do, you'll enjoy a $25 discount to your first purchase. And the way stitch fix works is pretty cool. I use it and have never been disappointed.
Tony [01:19:07]:
You'll set up a profile.
Tony [01:19:08]:
You'll put in all the sizes for your clothes as well as all the different brands and types of clothes that you like to wear. It's really simple and intuitive to set up. They'll show you pictures and pretty much give you a thumbs up or thumbs down option on if you would wear something or not. And you get to select all the brands that you already are used to wearing. With this information, there are thousands of passionate, trend setting stylists will curate a stitch fix box for you. They'll send you five items that you get to preview before they mail it to you, and you'll get to select based on the image if you like it or not. If not, they'll replace it with something else, and if so, they'll mail it to you absolutely for free. You can try everything on and you have a few days to send everything back or keep the stuff that you want to keep.
Tony [01:19:52]:
Then you can use that dollar 25 credit that I mentioned towards your purchase of those items. Again, to freshen up your wardrobe and also support the sponsor day podcast, go to sponsored a.com support and click on my affiliate link banner for Stitch fix and enjoy your $25 credit.
Tony [01:20:10]:
Do you want to start your own podcast?
Tony [01:20:13]:
Have a great show idea that you.
Tony [01:20:14]:
Want to get out into the masses but don't know quite how to get it from your head out into the world?
Tony [01:20:19]:
Well, here's how.
Tony [01:20:21]:
Use the podcast host Lipsyn. That's who I use to bring the sponsor Day podcast to you. Now you can use them the same way. Using the promo code spun spun, you can open up your lipsn account today and get two months of free podcast hosting.
Tony [01:20:39]:
Here's how it works.
Tony [01:20:40]:
Once you record your show, you upload it to your Lipsyn account where you can fill in your episode notes, upload your podcast art, and schedule when you want your episodes to release. Once you do that, Lipson will take care of the rest. They'll distribute your show to Spotify, Apple podcasts, YouTube, and all the other podcatchers that you choose instantaneously and seamlessly. Again, go to lipson.com and use the promo code spun spun to get two months free or use the affiliate link that's in the episode notes. Again, that's Lipson.com promo code Spun.
Tony [01:21:18]:
Take that great podcast idea from out.
Tony [01:21:20]:
Of your head and put it out into the world.
Tony [01:21:24]:
And as always folks, substitute the mysticism with hard work and start taking steps in the general direction of your dreams. Thanks for listening. I love you Aiden.
Zoila [01:21:48]:
I love you daddy.
Tony [01:21:50]:
I love you Grayson.
Tony [01:21:52]:
I love you daddy.